What is the most evidence-backed treatment in all of modern medicine? It’s not vaccines, or antibiotics, or even a healthy diet and regular exercise. Rather, it’s placebos, inert treatments that patients believe are the real thing. In the United States, every new medicine has to be tested against a placebo in order to be approved by the FDA. Consequently, every clinical trial provides additional evidence for the “placebo effect,” the phenomenon of placebos inducing significant healing responses. Yet, if placebos are simply sugar pills or sham surgeries, where do their healing effects come from? They come from us, and specifically, our thoughts, beliefs, and expectations about the treatment we think we’re receiving.
We are interested in understanding how these thoughts, beliefs, and expectations affect our health both within and beyond the realm of medicine, in domains such as exercise, diet, and stress. More specifically, we aim to isolate the mind’s influence on our health, explain how the mind influences health, and harness this influence, with the intent of improving public health and healthcare.
Below we dive into these three aims in greater detail, and highlight some of our ongoing and past research projects.

Aim 1: Isolate
One reason why the role of the mind in health is overlooked is simply that it’s difficult to study. Isolating the effects of our beliefs from the myriad of factors that influence our health is challenging. Our lab works to address these challenges by using creative methods to experimentally manipulate beliefs and expectations, and measure objective health outcomes.
In our work exploring the mind’s influence in shaping the benefits of exercise, we found that hotel housekeepers who were randomly assigned to learn that their work constitutes good exercise lost weight and had lower blood pressure compared to a control group who did not receive that information (Crum & Langer, 2007). Similarly, we have found that people who see themselves as less active than others have a significantly higher mortality risk 21 years later than those who see themselves as more active, controlling for actual activity levels (Zahrt & Crum, 2017).
We have also explored the mind’s influence in shaping physiological effects of food consumption. In one study, we had a group of participants drink identical milkshakes, but labelled some of the milkshakes as high-calorie and others as low-calorie. We found that participants who consumed the “high-calorie” milkshakes responded physiologically as if they had consumed more food, experiencing greater decreases in the hunger hormone ghrelin (Crum et al., 2011).
Our more recent work has showcased the role of the mind in shaping our genetic risk of disease (Turnwald et al., 2019). In another study, we analyzed participants’ genetic risk of obesity, and then randomly assigned them to receive either a ‘high-risk’ or ‘low risk’ genetic test result, independent of their actual risk. To test the effect of perceived risk, we compared physiological outcomes within individuals before and after being told their (randomly assigned) genetic risk. We found that informing individuals of high (versus low) genetic risk on a gene related to reduced exercise capacity had a self-fulfilling effect on their actual cardiorespiratory fitness during exercise. In other words, people who believed that they were at greater genetic risk for poor fitness experienced actual declines in their capacity to exercise.

Aim 2: Explain
But how do these subjective beliefs have objective effects on our weight, hormone levels, respiration, and other physiological outcomes? Our lab has worked to outline the pathways by which our minds can influence our health. One critical and often overlooked factor is that the body has a natural ability to heal itself with time, and our beliefs can evoke this healing response in the body. Our beliefs themselves are shaped by social and contextual factors such as physician characteristics, medical rituals, medicine branding, and cultural norms. Consequently, something as seemingly innocuous as the label on a milkshake can evoke physiological responses in the body by shaping our beliefs about the food we’re consuming.

This model reveals that placebo effects are not mysterious, unexplainable forces, but rather products of psychological and contextual factors that can be systematically measured and manipulated (Figure 1) (Crum, Leibowitz, & Verghese, 2017). For example, in one study (Howe, Goyer, & Crum, 2017) we manipulated both beliefs (by telling patients an inert cream would either boost or diminish their allergic reaction to histamine) and social context (by varying the doctor’s warmth and competence through verbal and nonverbal cues). We found that when a doctor conveyed cues of both warmth and competence, they elicited stronger placebo effects as measured by the size of the allergic reaction. Similarly, we’ve found that White patients show weakened responses to the placebo cream when their doctor is Black or female, illustrating how societal biases surrounding a provider’s race and gender may alter treatment outcomes (Howe et al., 2022).
Moreover, our lab has identified a certain class of beliefs that seem to be especially influential in shaping our health, which we term mindsets. Mindsets are core assumptions about aspects of the self and the world. Because mindsets are general beliefs as opposed to specific expectations, they tend to be stable across contexts and situations. For instance, you might see the stress you experience during a poker game as thrilling and work-related stress as exhausting, but what do you believe about stress in general? Is it enhancing or debilitating? Something to be avoided or utilized? The answers to these latter questions would constitute your stress mindset. Similarly, we might hold a mindset that healthy foods are fundamentally depriving (or indulgent), or that chronic illness is a catastrophe (or an opportunity).
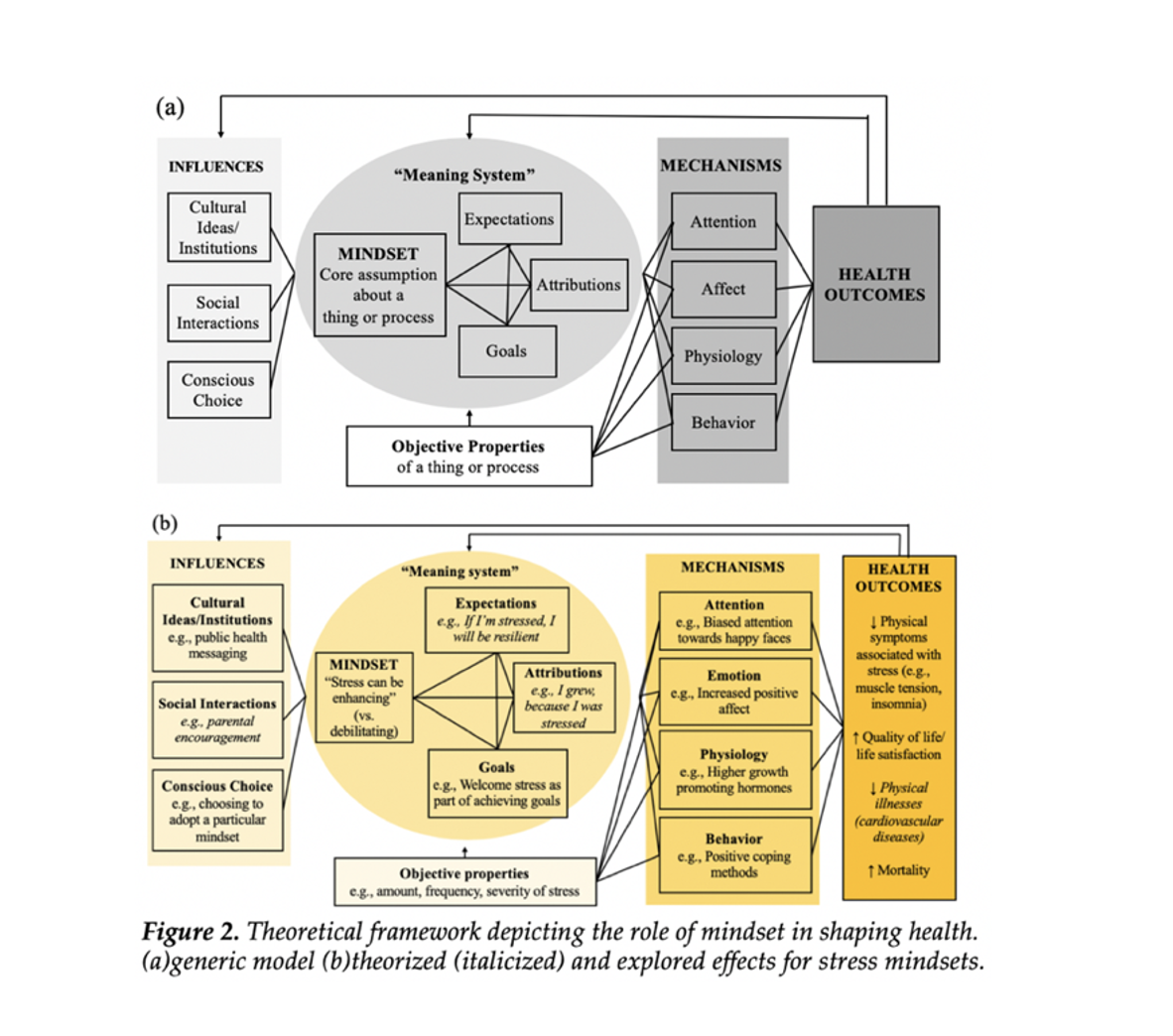
Because mindsets are consistent across contexts, they have more wide-ranging effects on our health than do situation-specific expectations. As shown in Figure 2, the mindset we hold toward a specific aspect of our health can change what we expect to happen (Expectations), why we think things are happening (Attributions), and what we want to happen (Goals). For example, people who see stress as enhancing (vs. debilitating) may expect to be resilient in the face of stressful circumstances, attribute personal growth to stressful experiences, and welcome stress as an inevitable part of achieving their goals. This set of beliefs then influences what we pay attention to, how we feel, what we do, and our physiology. In the case of stress, we might experience more positive emotions, be more inclined to pay attention to others who are thriving, use more positive coping methods for dealing with stress, and even secrete more growth-promoting hormones. All of this adds up to markedly different health outcomes between people who see stress as enhancing vs. debilitating, with the former experiencing less muscle tension and insomnia, higher quality of life, and lower risk of cardiovascular disease.
Moreover, the framework in Figure 2 illustrates how mindsets and their meaning systems are shaped by our cultures and social interactions, as well as by our own conscious choice (more on that later). Altogether, our health is co-created by our subjective mindsets and the objective properties of the domains our mindsets are about (e.g., aging, diet, stress, illness, and treatment). The generic framework (Panel A) can be applied to a wide-variety of different mindsets. Panel B showcases the theorized (italics) and explored effects in the context of mindsets about stress.

Aim 3: Harness
So if mindsets are so powerful, how can we harness this power to become healthier and happier? Increasingly, our lab is focused on identifying mindsets that may be especially beneficial for our health, and developing interventions to help people adopt those mindsets. Our research on stress mindset shows that delivering vivid, persuasive, and actionable information about the potentially enhancing effects of stress can help establish the mindset that “stress can be enhancing” and, in turn, improve health (see Figure 2 above) (Crum, Salovey, & Achor, 2013; Crum et al., 2017). Similarly, our research on food mindsets suggests that altering public health messaging to establish the mindset that “healthy foods can be indulgent and delicious” may be a more effective route for improving health and motivating healthy behaviors than messaging that harps on the importance of eating healthily (which can inadvertently reinforce a mindset that “healthy foods are depriving/disgusting”) (Turnwald et al., 2017; Turnwald et al., 2019). In several studies (Turnwald, Boles, & Crum, 2017; Turnwald et al., 2019; Turnwald & Crum, 2019), we’ve found that labeling vegetables with tasty and indulgent descriptors led to a 29-40% increase in consumption compared to highlighting their health characteristics. Relatedly, our research on exercise mindsets has yielded several important insights for making physical activity guidelines more effective (Zahrt & Crum, 2020).
My lab also partners with medical teams to design and implement randomized controlled trials that improve treatment experience and outcomes by instilling more adaptive mindsets. In one study (Howe et al., 2019) we improved the outcomes of children going though Oral Immunotherapy Treatment (OIT) for peanut allergies by altering their mindsets about side-effects associated with the treatment. Half of the participants were randomized to receive a typical warning message: side effects are negative outcomes that need to be managed and endured. The other half were given messages to instill the mindset that some mild symptoms are often a sign that the treatment is working (which is true in Oral Immunotherapy Treatment). Compared with families informed that symptoms are negative side effects, families informed that “symptoms are positive signs of treatment efficacy” experienced significantly less anxiety, fewer symptoms during the highest doses, and improved IgG4 levels, an immune marker of allergic tolerance. This study suggests we can inform patients about side effects without exacerbating them and is representative of the vast potential for similar studies to test mindset interventions in healthcare. Our current work includes developing and testing mindset interventions for cancer patients, people living with osteoarthritis, older adults, and people dealing with long-term outcomes from the COVID-19 pandemic.